Three out of four healthcare executives identify data interoperability as a top priority—and for good reason. Secure, real-time data exchange across healthcare systems streamlines processes like claims routing, enhances decision-making by providing timely access to consumer information, and ensures compliance with CMS and ONC requirements.
Is your enterprise ready to harness the power of interoperability? In this blog, we explore how seamless data exchange can optimize operations, drive better outcomes, and position your enterprise for long-term success.
Healthcare Data Interoperability
Data interoperability in healthcare simply refers to the ability of healthcare systems to seamlessly exchange and use health information without disrupting operations or compromising data security. Whether shared within departments or across enterprises, interoperability ensures that critical information moves safely and accurately across the entire care continuum.
Benefits of Data Interoperability in Healthcare
Every healthcare stakeholder has distinct goals when working with data, and data interoperability is vital in helping them achieve these goals. Below are the key benefits of interoperability for healthcare enterprises :
- Elevated Care Experiences : Interoperability allows healthcare enterprises to have seamless access to a patient’s or member’s complete health history, enabling more informed decision-making and improved care delivery.
- Improved Care Coordination : Real-time data sharing between healthcare enterprises reduces redundancy, minimizes the risk of errors, and ensures that all stakeholders have up-to-date, accurate information for better-coordinated and more efficient care delivery.
- Optimized Business Operations : By streamlining data exchanges, interoperability reduces administrative burdens, minimizes manual processes, and enhances overall productivity. This allows healthcare enterprises to focus more on delivering high-quality care and less on operational hurdles.
- Streamlined Claims Processing : Interoperability accelerates claims processing by automating data exchange and reducing manual work. This helps prevent errors and delays, improves cash flow, and makes operations more efficient.
- Better Risk Management : With real-time access to comprehensive and accurate data, healthcare enterprises can more effectively identify, assess, and mitigate potential risks.
- Cost Reduction : Seamless data sharing helps eliminate unnecessary procedures, reduce administrative overhead, and optimize resource utilization, leading to serious cost savings across the healthcare ecosystem.
Barriers to Effective Healthcare Data Exchange
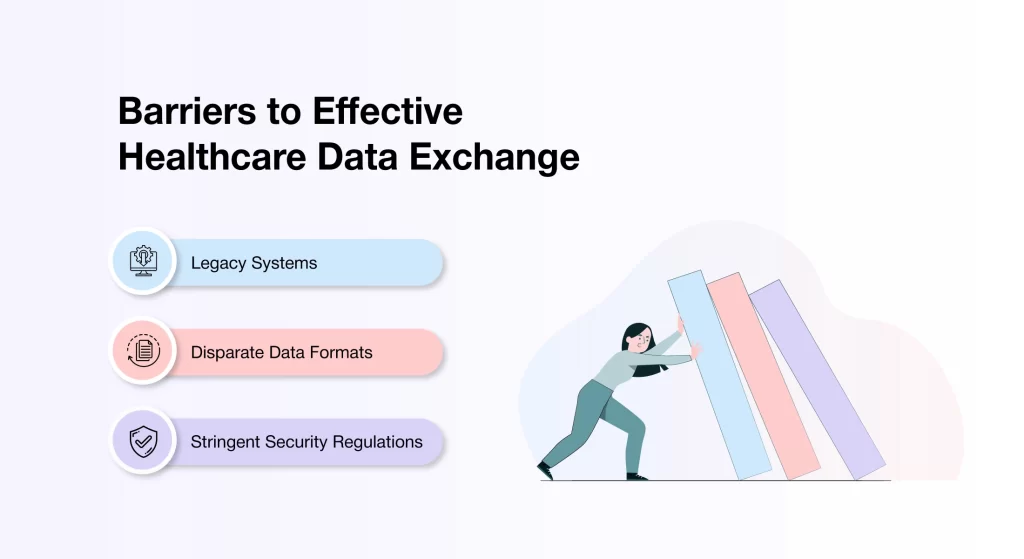
Healthcare enterprises rely on traditional systems such as Health Information Exchanges (HIEs) and Electronic Health Records (EHRs) to manage operational data. However, the varying transmission standards and data formats used by these systems create significant barriers to seamless data exchange between enterprises.
- Legacy Systems: Many healthcare enterprises continue to rely on legacy systems that were not built to meet modern data-sharing requirements. These outdated platforms often lack healthcare API integration and real-time integration capabilities, making seamless data exchange a challenge.
- Disparate Data Formats: Healthcare systems often record and encode the same data in different formats. For example, one system may use a specific code for a diagnosis, while another uses a completely different one. This lack of standardization complicates data sharing and hinders interoperability.
- Stringent Security Regulations: Healthcare data is inherently sensitive and thus requires robust data protection. However, adhering to extensive security regulations while enabling data sharing can create delays. Achieving a balance between securing data and ensuring real-time access remains a critical challenge.
Overcoming Common Barriers To Interoperability
While healthcare interoperability brings substantial advantages to both payers and providers, implementing it often presents various challenges. Below are some effective strategies enterprises use to overcome these barriers and achieve successful interoperability :
Modernize Legacy Systems
Many healthcare enterprises still rely on outdated systems that lack compatibility with modern technologies. Upgrading these systems can be complex, especially when trying to avoid disruptions to daily operations. A phased approach—combining incremental system enhancements with comprehensive staff training—can ease the transition, support long-term interoperability, and minimize workflow interruptions.
Prioritize Data Security
Ensuring security of sensitive healthcare data is a foundational step toward achieving interoperability. Today, enterprises are adopting robust measures—such as advanced encryption, role-based access controls, and continuous security monitoring—to protect critical healthcare information during data exchange. These safeguards reduces the risk of breaches and ensure compliance with regulatory standards and foster greater trust among stakeholders.
Adapt to Evolving Regulations
The regulatory landscape in healthcare is constantly evolving, with new data standards and compliance requirements emerging regularly. To ensure ongoing compliance, enterprises must conduct regular audits, update internal policies, and make necessary adjustments to their data exchange frameworks. A proactive approach to monitoring regulatory shifts not only ensures secure and lawful data exchange but also mitigates the risk of costly compliance violations.
Steps to Implement Healthcare Data Interoperability
To successfully implement healthcare interoperability, enterprises must follow the following key steps :
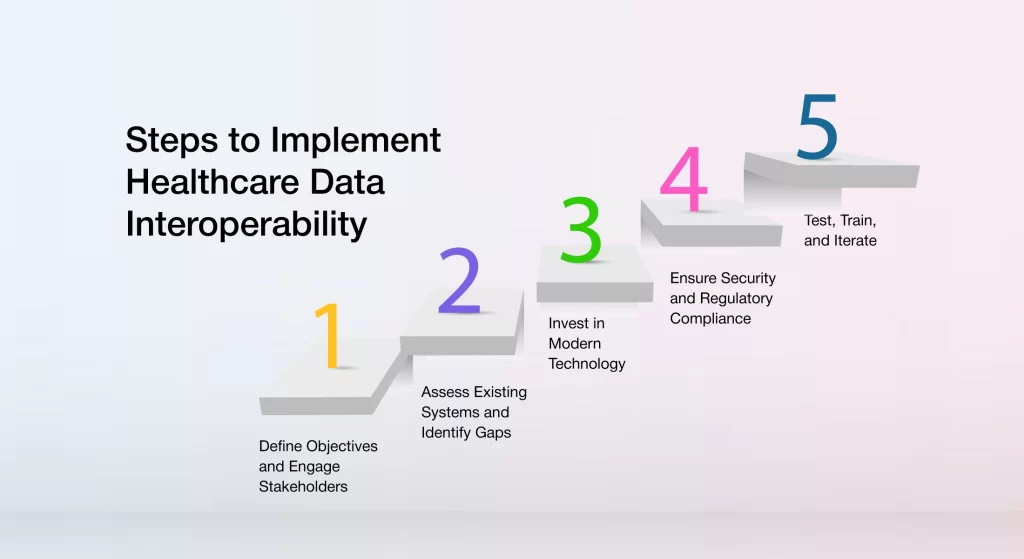
Define Objectives and Engage Stakeholders
The first step in implementing healthcare data interoperability is to establish clear goals and engage all key stakeholders—clinicians, IT teams, payers, and administrative staff—from the outset. Involving everyone early in the process ensures alignment on objectives, promotes collaboration, and enables the development of a detailed, unified roadmap. This proactive approach makes sure that all stakeholders are on the same page, laying the groundwork for a successful and coordinated implementation.
Assess Existing Systems and Identify Gaps
Next, enterprises must evaluate their current IT infrastructure and data workflows. This includes reviewing legacy systems, data silos, and any areas where information exchange is inefficient or lacking. By identifying these gaps, enterprises can pinpoint the necessary updates or integrations required to enable seamless data sharing and enhance interoperability across the organization.
Invest in Modern Technology
Adopting the latest healthcare technologies is essential for achieving interoperability. Enterprises should select tools and platforms that support standardized data formats and enable secure, real-time data sharing. Cloud-based solutions, scalable APIs and integration platforms can help unify disparate systems and improve data accessibility across the board.
Ensure Security and Regulatory Compliance
Safeguarding sensitive healthcare data during exchange is essential for maintaining trust and achieving successful interoperability. Enterprises should always implement robust security measures, such as advanced encryption, role-based access controls, and regular compliance audits, to ensure data integrity. Additionally, all systems must align with evolving regulatory requirements to protect patient and member privacy.
Test, Train, and Iterate
Before full-scale deployment, enterprises should run pilot programs to assess system performance in real-world scenarios. Along with providing comprehensive training to teams for seamless adoption, it’s crucial to gather and analyze user feedback to pinpoint areas for improvement. By continuously refining the system based on these insights, enterprises can ensure it’s sustained effectiveness and adaptability in the long term.
Future Trends in Healthcare Data Interoperability
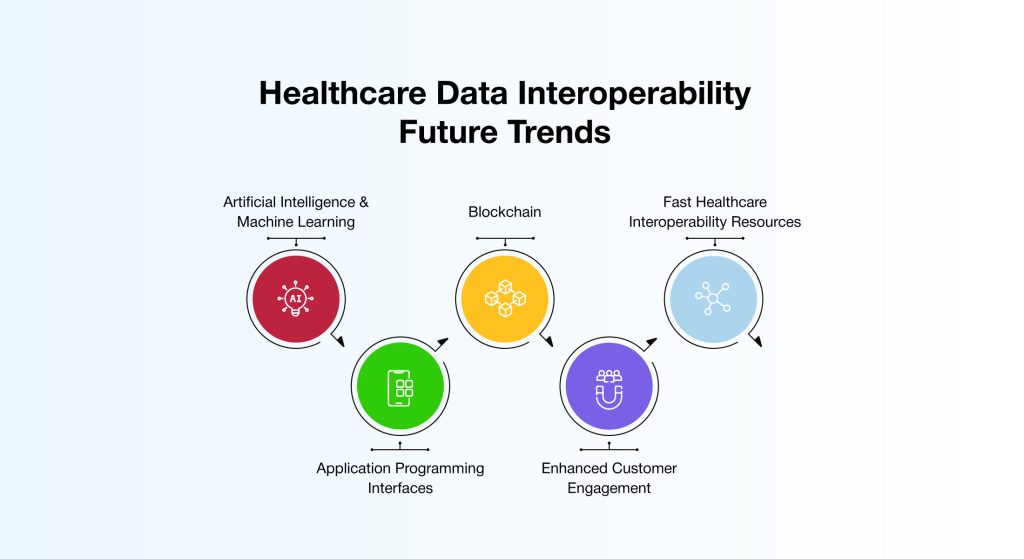
Outdated data exchange methods and persistent data silos continue to hinder efficiency and collaboration across the healthcare landscape. To address these challenges, enterprises are embracing modern, future-ready solutions that promote seamless and secure data sharing. Below are some of the key innovations and trends shaping the future of healthcare data interoperability :
Artificial Intelligence & Machine Learning
AI and machine learning are transforming how healthcare data is standardized and shared. These technologies automatically classify unstructured EHR data and map it to FHIR standards, enabling real-time decision support. Furthermore, AI-driven tools are increasingly being used to harmonize and integrate disparate data formats across EHRs, payer systems, and provider networks, minimizing manual intervention and reducing errors.
Blockchain
Blockchain is transforming healthcare data security and interoperability. Emerging applications, such as self-sovereign identity (SSI), empower individuals to directly control access to their health data without relying on intermediaries. Additionally, federated blockchain networks facilitate secure collaboration between hospitals, insurers, and third-party administrators, ensuring data privacy while enhancing transparency and interoperability.
Fast Healthcare Interoperability Resources (FHIR)
FHIR is a set of standards designed to simplify and secure healthcare data exchange. By providing a flexible framework for exchanging health information, FHIR facilitates integration across diverse healthcare systems while making sure compliance with privacy regulations and security protocols.
Application Programming Interfaces (APIs)
The challenge of data silos and isolated systems in healthcare is being addressed through customizable APIs. By establishing specific protocols for data exchange, APIs enable seamless communication between healthcare systems.
Enhanced Customer Engagement
By empowering patients/members with a secure, real-time access to their health data, enterprises allow them to actively participate in their care. Advanced consumer portals, AI-driven health insights, and wearable device integrations allow individuals to track their health history, monitor vital signs, and make informed health decisions.
Real Life Case Study
AVIZVA, a leading healthcare technology company, partnered with Aflac Benefits Solutions (ABS), a prominent third-party administrator (TPA), to tackle the complexities of healthcare data interoperability.
With nearly 1 million dental and vision members to serve, ABS has to collaborate with several external service providers. Each of these partnerships involves the efficient and secure exchange of critical healthcare data between ABS core systems and external partner systems. This data exchange is inherently complex due to the disparate nature of both the data and the systems involved.
The healthcare data varies significantly in structure and format, while the partner systems are distinct, operating independently with no unified industry standard. Consequently, the integration process must address variability across multiple service partners, each with unique systems and large volumes of unstructured or semi-structured data.
To overcome these complexities of disparate data exchange, AVIZVA conceptualized and engineered an intelligent data connectivity solution for ABS. By offering secure, and seamless data exchange across disparate systems, the future-ready solution made it easier for ABS to scale and onboard new partners quickly.
Key features of the solution include centralized member profiles, real-time prescription tracking, and self-service tools for prescription renewals and drug pricing. With this data connectivity solution, ABS now manages over 5 million prescriptions, processes 30 million claims annually, and offers enhanced member engagement.
This case demonstrates how payers and providers can effectively overcome interoperability challenges through innovative, cutting-edge solutions, driving both operational efficiency and improved consumer experiences.
AVIZVA : Redefining The Future of Healthcare Data Interoperability
AVIZVA is a healthcare technology company that empowers payers, TPAs, and PBMs to accelerate, simplify, and optimize care delivery. By offering next-generation interoperability solutions, AVIZVA helps enterprises streamline data exchange across systems while ensuring compliance with evolving regulatory requirements. Here’s what sets AVIZVA’s interoperability approach apart :
AI-Driven Data Standardization & Integration
Healthcare data is often fragmented across different formats and platforms, making seamless interoperability a significant challenge. AVIZVA leverages advanced AI technologies to intelligently standardize, normalize, and map data across FHIR, HL7, EDI, and custom formats. This enables secure, consistent, and efficient data exchange between systems, providers, and payers, laying the groundwork for unified healthcare customer experiences.
Unified Interoperability Hub
The interoperability solutions offered by AVIZVA serve as centralized hubs connecting EHRs, payer systems, provider networks, and third-party platforms. The solutions facilitate real-time data synchronization, validation, and access, streamlining critical processes like claims management, eligibility verification, and prior authorizations. By eliminating manual inefficiencies and delays, AVIZVA helps enterprises accelerate workflows and improve decision-making.
Secure & Compliant Data Exchange
Security and compliance are at the core of AVIZVA’s interoperability framework. The platforms ensure end-to-end data protection through robust encryption, role-based access controls, and secure, API-based exchanges. They further adhere to HIPAA, CMS interoperability rules, and ONC standards, giving enterprises the confidence to share sensitive health information without compromising on privacy or regulatory compliance.
Automated Prior Authorizations & Claims Processing
AVIZVA’s interoperability solutions significantly minimize manual intervention in critical processes such as prior authorizations and claims processing. By automating eligibility verification, authorization requests, and real-time claims adjudication, these solutions reduce administrative overhead and expedite reimbursements.
Interoperability-Ready Consumer & Provider Portals
AVIZVA offers FHIR-based consumer access APIs and provider collaboration platforms, enabling the seamless sharing of health records, claims history, and benefits. The intuitive portals foster better engagement, reduce friction, and ultimately improve healthcare outcomes.
Conclusion
Siloed healthcare systems create substantial operational challenges and heighten the risk of errors and security breaches, including unauthorized access to sensitive data. Therefore, data interoperability is crucial not only for meeting regulatory requirements but also for enabling a secure, real-time data exchange environment. By leveraging intelligent interoperability solutions, TPAs and PBMs can make well-informed, accurate decisions, leading to improved healthcare outcomes and enhanced operational efficiency.
AVIZVA is a leading healthcare technology company that empowers Payers, TPAs and PBMs with future-proof interoperability solutions. With 14 years of industry expertise, AVIZVA offers a complete range of solutions that are designed to address various business needs, including data integration, exchange, synchronization, and more.
Ready to transform your interoperability strategy? Get in touch with AVIZVA today!