A Suite of AI Enabled Web Portals & Native Mobile Applications for Your Stakeholders & Consumers
Purpose-built for the Modern Needs of Payers, TPAs, and PBMs
Intelligent Portals Designed for Experience, Engagement & Efficiency.
Advanced technology and human-centered design that engage consumers deeply, empower seamless self-service, and streamline complex operations. All while improving health outcomes and giving Payers the agility to scale for the future.
Design
Human-centered, intuitive interfaces that make complex healthcare interactions simple for every user.
Technology
Scalable, AI-powered, and compliance-ready platforms built on modern architecture for tomorrow’s needs.
Enhances Engagement
Keeps all stakeholders actively connected through smart campaigns, notifications, and multi-channel experiences.
Promotes Self Service
Empowers every user to manage benefits, claims, and care independently, reducing support calls and delays.
Streamlining Operations
Automates workflows, integrates data seamlessly, and cuts through administrative complexity for faster outcomes.
Elevate Your Consumer Experience
By Combining Conversational & Predictive Intelligence
For Seamless Personalized Engagement
Elevate your consumer experience by offering a dynamic, personalized portal solution that understands and anticipates customer needs, ensuring seamless engagement at every touchpoint. Through real-time conversations and proactive recommendations, empower your business to forge deeper, more meaningful connections, cultivating lasting loyalty and exceptional satisfaction.
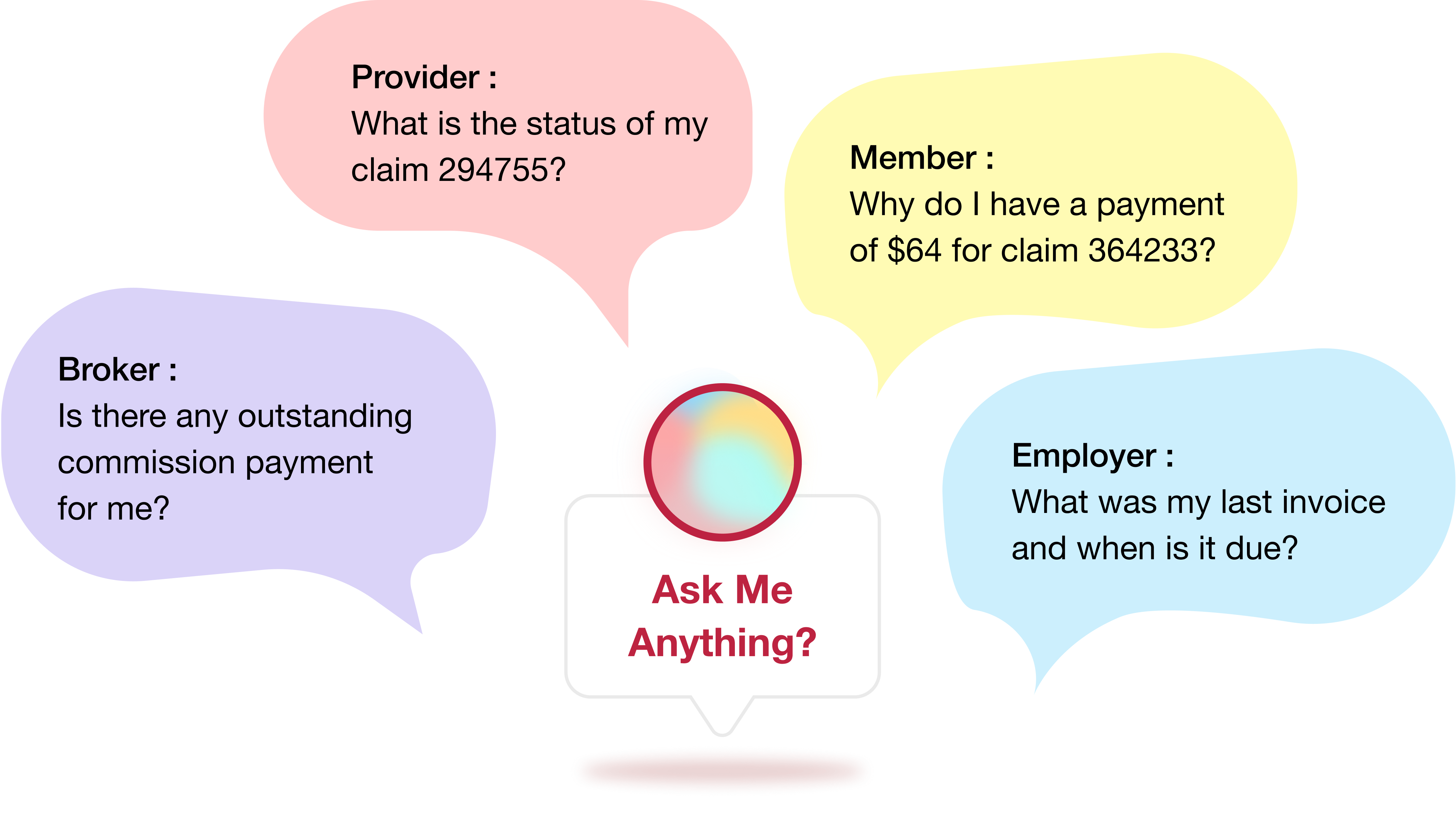
Intelligent Features That Are Seamlessly Integrated Across All Portals
- End-to-End Transparency Across Workflows
- Multi-Channel Access (Web, Mobile, Messaging, Phone)

Dive Into the Capabilities of Feature-Rich Portals
Empowering Every Consumer
Designed to Enhance Your Member Engagement, Drive Better Health Outcomes & Reduce Care Delivery Efforts
A One Stop Shop for Members to manage their coverage, search for benefits, find care, understand claims, and track prior authorizations. While it primarily focuses on enabling ease of self-service, thereby reducing operational workload for enterprises, it also simplifies and enhances interactions with Member Engagement teams.



Tools, Insights, and Transparency At Every Stage of Interaction With Payers
Empowering Providers at every step of their interaction with Payers — Pre-Service, During Service, and Post-Adjudication - by providing them with the tools, insights, and transparency they need to focus on what matters most: patient care.



Transforming Benefits Administration for your Employers with Efficiency, Engagement, Insight, and Cost Control
With the needs of employers in mind, the platform is designed to allow effortless management and oversight of employee benefits and usage. Employers can easily manage their group membership, including open enrollment, life change events, member profile information, understanding plan benefits, invoices, and plan performance.



Empowering Brokers with Full Control, Insight, and Efficiency for better client acquisition and retention.
Designed to simplify Client Acquisition, Management & Retention for Agencies & Agents. It brings capabilities to manage the entire lifecycle of clients, covering pre-sales, sales, and post-sales at fingertips. Some of the most used and high-impact features include quoting and proposals, managing their book of business, accessing commission statements, and gaining ready access to insightful analytics.



Designed to Elevate Your Consumer Engagement Strategy
Unlock The Power of Integrated Self-Service, Automation, Conversational AI, and Omnichannel Access
Discover how it all works in a tailored demo experience!
Schedule Now
Are You An Enterprise Evaluation Build or Buy?
We Can Help You Navigate Your Dilemma By Offering You The Best Of Both Worlds


