In today’s healthcare landscape, data is both an opportunity and a challenge. With vast volumes of member information, claims records, notes, and compliance mandates flooding in every second, health insurers are tasked with turning this data deluge into timely, actionable insight.
But legacy analytics systems can’t keep up.
The result? Slower decision-making, missed fraud signals, rising costs, and delayed care — all of which erode trust and efficiency across the insurance value chain.
Enter the next era of healthcare analytics, powered by artificial intelligence.
From generative AI that drafts personalized plan summaries in seconds to predictive algorithms that flag potential fraud before a dollar is lost, health insurers are embracing intelligent analytics to drive smarter, faster, and more transparent decisions. And the impact is enormous — just in fraud detection alone, AI is helping insurers address an issue that drains the U.S. healthcare system by as much as $230 billion annually.
This blog explores why traditional health insurance analytics need a reboot, and how AI is stepping in to redefine outcomes for insurers, members, providers, and employers alike.
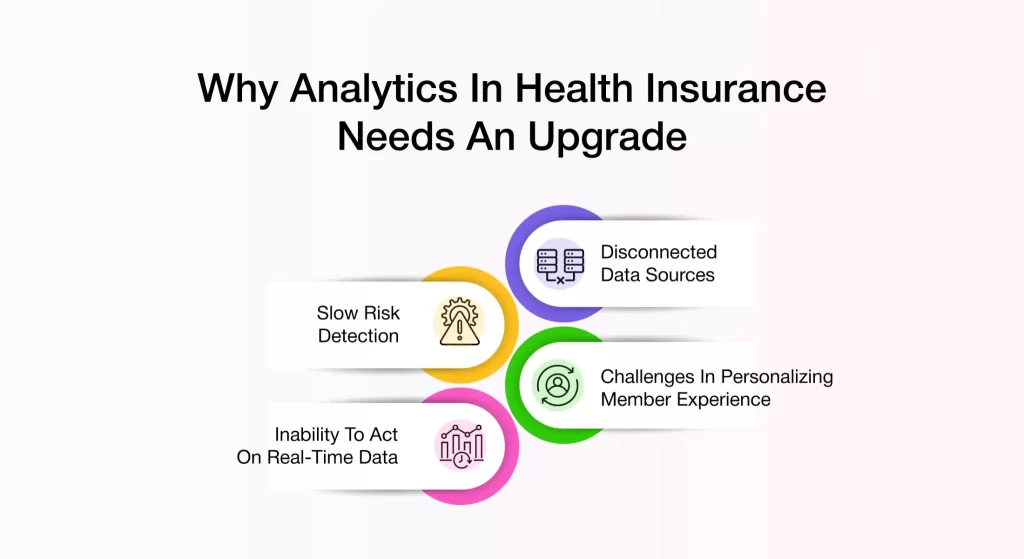
Why Analytics in Health Insurance Needs an Upgrade
In today’s dynamic healthcare landscape, analytics isn’t just a back-office tool — it’s a strategic driver of smarter decisions, improved member experiences, and proactive risk mitigation. Yet, many health insurance enterprises are still grappling with outdated analytical frameworks that fall short of supporting modern demands.
However, there are still some challenges that stop the industry from gaining these full benefits. The following factors highlight the key obstacles preventing health insurers from unlocking the full potential of analytics.
- Disconnected data sources
- Slow risk detection
- Challenges in personalizing member experience
- Inability to act on real-time data
Let’s understand these points in detail.
Disconnected Data Sources
Member data is often fragmented across disparate systems — from claims and health records to wearable devices and call center logs. Without a unified data foundation, insurers struggle to derive meaningful insights.
Delayed Risk Detection
Traditional rule-based systems typically flag issues after they’ve occurred. By the time fraud is caught or a member’s condition escalates, it’s often too late to intervene effectively.
Limited Scope in Personalization
Generic messaging and one-size-fits-all care programs miss the mark in an era where members expect hyper-personalized support based on their unique health journeys and preferences.
Inability to Act on Real-Time Data
Most traditional analytics systems were built for retrospective reporting — not real-time responsiveness.
In a fast-moving healthcare ecosystem, this delay can be costly. Whether it’s identifying a high-risk member requiring intervention or detecting suspicious claim activity, insurers need analytics platforms that can ingest, interpret, and act on data instantly to stay ahead of the curve.
Inefficiencies in Operational Processes
Outdated analytics infrastructure slows down critical workflows like claims processing, prior authorizations, member onboarding, and support. The result? Increased turnaround times, higher administrative costs, and inconsistent service quality. Without intelligent automation and advanced analytics, operational teams are forced to rely on reactive processes instead of proactive strategies.
Missed Opportunities for Predictive Insights
Without access to sophisticated predictive models, health insurers miss out on key strategic advantages. AI-powered analytics can identify patterns before they escalate into costly issues — from preventing chronic condition flare-ups to forecasting enrollment behavior. Predictive insights allow insurers to allocate resources more effectively, manage risk dynamically, and enhance cost control — all while delivering personalized, anticipatory care experiences.
AI Transforming Health Insurance Analytics
AI in health insurance is projected to generate a $164.16 billion market value by 2030. AI is transforming health insurance services through its ability to deliver exceptional growth across the industry. AI demonstrates its considerable value through automatic processes and its ability to identify irregularities in insurance management systems.
Traditionally seen as a back-office enabler for automation and fraud detection, AI has now emerged as a strategic engine powering smarter decisions, faster service delivery, and personalized member experiences. Health insurers are increasingly leveraging AI to make sense of complex data environments, anticipate member needs, and optimize operational performance.
Here are three powerful ways AI is delivering impact across the healthcare insurance value chain:
- Predictive analytics
- Real-time insights
- Automated Decision Support
Let’s understand these in detail.
Predictive Analytics
AI models can forecast everything from disease progression to potential claim volumes. These insights allow insurers to proactively manage high-risk members, prevent costly hospitalizations, and fine-tune plan design to meet evolving member needs.
Here’s how AI is making a significant impact:
- Forecasting Claim Volume
AI-powered claim management software uses historical claims data and external factors like seasonal changes, economic shifts, and demographic trends to predict future claim volumes. AI in health insurance claims allows you to prepare for periods of high claims, optimize your resources, and streamline claims processing.
- Chronic Disease Trend Prediction
AI-powered predictive models analyze patterns in member health data to identify early signs of chronic diseases, such as diabetes or heart disease. By forecasting the likelihood of chronic conditions developing, insurers can take a proactive approach in managing member health..
- Member Churn Forecasting
AI doesn’t just improve operational efficiency—it also safeguards revenue.
AI in health insurance can predict when members are likely to leave or switch providers by analyzing factors like claims history, satisfaction levels, and service usage. By identifying at-risk members early, insurers can implement retention strategies, offer personalized benefits, and improve customer engagement to reduce churn.
Real-Time Insights
In the high-stakes world of health insurance, decisions made in real time can mean the difference between mitigating risk and missing opportunities. .
Immediate Fraud Detection
Gone are the days of discovering fraudulent claims after the damage is done. Traditional fraud detection methods relied heavily on historical data and manual review processes, which can take weeks or even months to identify suspicious claims. With AI in health insurance, insurers can now analyze claims data on the fly, flagging suspicious patterns, unusual billing behaviors, or outlier claims as they occur. By eliminating delays and reducing reliance on manual review, insurers can stop fraud in its tracks, saving millions and maintaining the integrity of their operations.
Provider Performance Monitoring
Another significant application of generative AI in health insurance is monitoring the performance of healthcare providers in real time. AI can process data from various sources, such as claims, patient satisfaction surveys, and treatment outcomes, to evaluate how well providers are delivering care. This allows health insurance companies to understand how providers perform, how efficient they are, and how well they follow standard practices. They can use this information to make decisions about their provider networks, plan improvement efforts, and negotiate better contracts. Ultimately, this leads to improved care for members, lower costs, and stronger provider partnerships.
Automated Decision Support
In a landscape as dynamic and regulation-heavy as healthcare insurance, decision-making speed and accuracy are critical.
With AI’s automation features, for instance, AI claims automation, health insurers make critical decisions, particularly around pricing, coverage limits, and risk selection, more effectively and on time. Here’s how AI is transforming this aspect of health insurance:
1. Intelligent Underwriting: AI algorithms analyze vast data sources—from historical claims to lifestyle patterns and social determinants of health—to assess risk more accurately and instantly. This enables faster policy issuance, minimizes human bias, and enhances pricing precision, all while improving customer satisfaction through a frictionless experience.
2. Claims Adjudication & Processing: Traditionally time-consuming and prone to error, claims processing is now streamlined through AI. By automating claim reviews, validations, and payout decisions, insurers can reduce turnaround times, lower administrative costs, and ensure regulatory compliance—with fewer errors and less manual intervention.
3. Personalized Plan Recommendations: AI doesn’t just process data—it understands it. With real-time behavioral and historical data at its fingertips, AI systems can match members with the most relevant health plans, tailored to their needs, usage patterns, and risk profiles. The result? Higher member engagement, increased retention, and better health outcomes
AVIZVA: AI Partner for Health Insurance Companies
AVIZVA is a leading healthcare technology company dedicated to empowering payers, TPAs, and PBMs to streamline and enhance care delivery through advanced AI-driven solutions. With over 14 years of specialized healthcare experience, AVIZVA delivers a comprehensive suite of services and proprietary products designed to meet the evolving needs of the industry.
Supported by a strong history of client partnerships and more than 150 custom product implementations, AVIZVA stands as a trusted partner for healthcare enterprises seeking innovation and operational excellence.
Introducing VIZCare Copilot — AVIZVA’s intelligent healthcare AI assistant designed to seamlessly integrate AI into business operations. Key capabilities include:
- Personalized self-service interactions tailored for all healthcare stakeholders, including members, providers, brokers, and employers, leveraging sophisticated AI to enhance engagement and satisfaction.
- AI-powered automation and support for internal teams, reducing manual tasks and enabling faster, more precise service delivery.
- Robust interoperability with existing healthcare platforms and systems, ensuring seamless integration without disrupting current workflows.
- Embedded healthcare intelligence engineered to address industry-specific complexities and regulatory requirements with accuracy.
- Comprehensive compliance with HIPAA and PHI standards, guaranteeing data security and privacy at every interaction point.
AVIZVA delivers proven, scalable AI solutions that drive operational efficiency, improve stakeholder experience, and maintain rigorous compliance, making it the ideal technology partner for healthcare organizations ready to embrace digital transformation.

Conclusion
In today’s AI-driven market, not having AI solutions in healthcare is not a choice but a necessity. AI is transforming the health insurance industry by providing faster, more accurate insights that drive better decision-making and operational efficiency. With AI-driven analytics, such as predictive analytics, insurers can enhance their customer service offerings, reduce fraud, and improve customer satisfaction.
By leveraging AI tools like AVIZVA’s VIZCare Empower platform, health insurance companies can streamline operations, personalize member experiences, and stay competitive in a rapidly evolving market. Embracing AI in health insurance is no longer a luxury; it’s a necessity for future success.
Curious to see how AVIZVA can transform your healthcare workflows? Let’s talk—schedule a call with us today!