
An Evolving Journey Of Technology-Driven Modernization
The Context
Imagine 360 was founded in 2022 when EBMS, ELAP Services, and Group & Pension Administrators (GPA TPA) joined forces, bringing together their decades of expertise to redefine self-funded plans. Since then, Imagine 360 has consistently integrated reference-based pricing with enhanced benefits administration & dedicated member support, establishing itself as an industry leader in delivering cost-effective, high-quality healthcare solutions.
Our association with EBMS, however, dates back long before the formation of Imagine360. As an independent pioneer in self-funded health plan administration since 1980, EBMS led the way with groundbreaking innovations – introducing independent employer clinics and wholesale pharmaceutical benefits – that reshaped how businesses managed healthcare costs.
In 2017, EBMS accelerated its transformation and expanded its technological capabilities by partnering with Water Street Healthcare Partners. This pivotal partnership set the stage for the formation of Imagine360, where the collective expertise of three enterprises continue to drive improvements in the cost, quality, and overall experience of healthcare for both employers and their employees.
The Business Need
Through every stage of this evolution, Imagine360 has strengthened it’s partnership with us. From relying on our expertise to support EBMS in its independent years to empowering us with a key role in Imagine360’s rise as an industry leader, they have consistently entrusted us to drive innovation, optimize healthcare access, and deliver greater cost efficiencies.
Business Growth
- Flexibility to Add New Sales Channels
- Ability to Add Partners for Growth and Enhance Customer Offerings
Enhanced Customer Experience
- Modern and assistive self service channels
- Simplified and easy access to care and benefits
Efficient Scalability
- Automation of business processes
- Replacement of legacy technology that restricts flexibility with modern platforms that can easily adapt to changing business needs
Security and Compliance
- Improved data security measures spanning encryption & firewalls
- Protection against cyber threats and data breaches
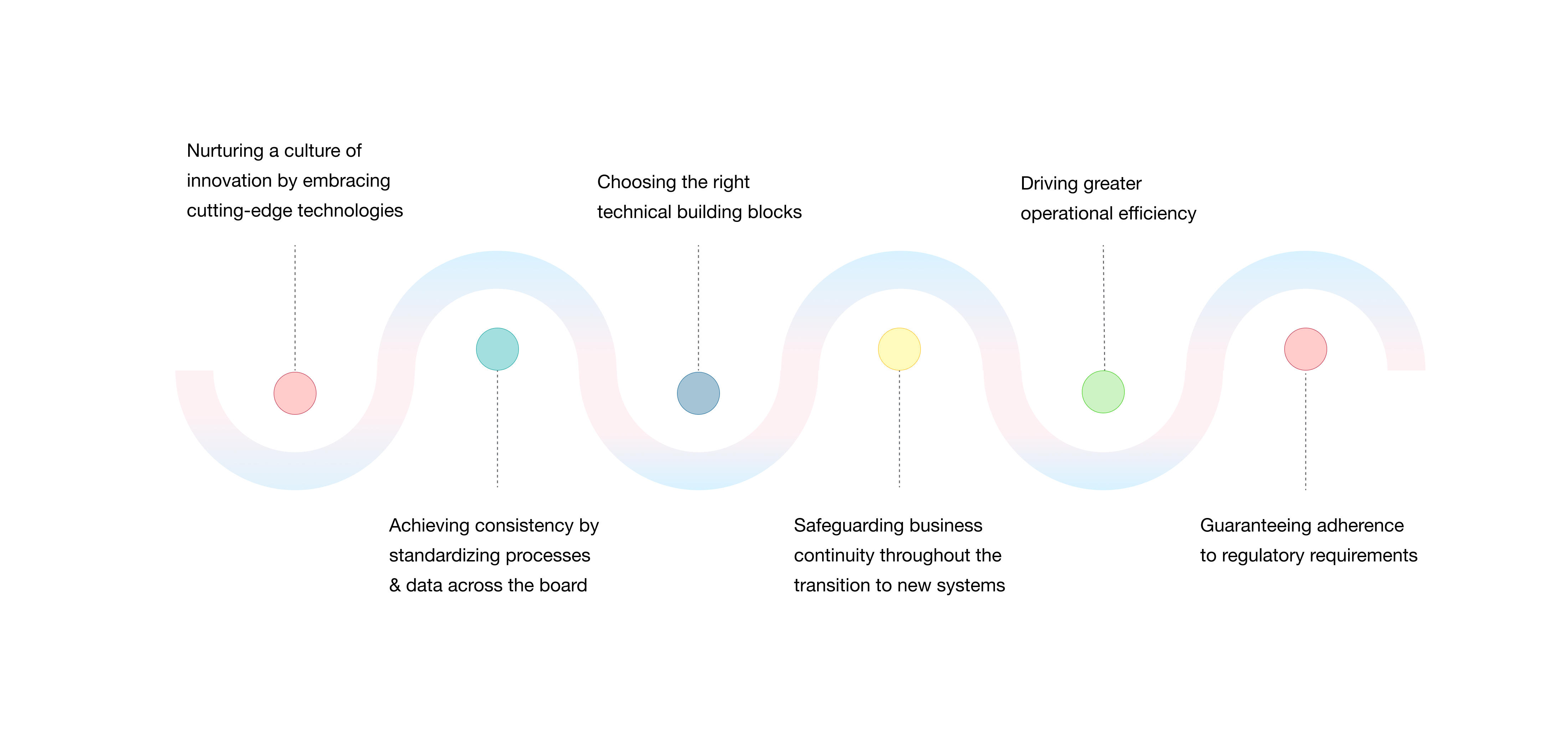
Our Approach to Transformation
While defining the transformation roadmap, we focused on leveraging scalable, forward-looking technologies and migrate to systems that offered intuitive, user-friendly interfaces.

The Journey
Year 01
Year 01
Foundation Setup :
Defined the Technology Stack, Design Patterns, and and Cloud Adoption Strategy to facilitate the transition from a fully on-premises infrastructure to a cloud based environment.
Key considerations :
Performance, Scalability, Flexibility, Future-Proofing, and Development Speed.
Initiatives :
- Migrated a subset of business from Legacy Claim Processing Platform to A Modern Claim System
- Developed a new Data Integration platform that streamlines integration with internal and external systems integration, enabling efficient movement of eligibility data within and outside the organization
- Spearheaded the cloud deployment of a modern, revamped Member Experience
Key Achievements
- Built confidence in migrating business to a new claims system, overcoming what was initially seen as a significant challenge
- Increased auto-adjudication rates for migrated groups, reducing the need for manual intervention
Year 02
Year 02
Initiatives :
- Migrated a bulk of business from legacy claim processing platform to new/modern claim system
- Relocated inbound and outbound data feeds from legacy technology to the New Data Integration platform. This included additional data types such as Claims and Accumulators
- Successfully deployed a modern, revamped Employer Experience
Key Achievements
- Boosted auto-adjudication rates as a larger volume of business was migrated to the new claims system
- Reduced turnaround time for data exchanges with vendors while enhancing reliability
- Strengthened market position by expanding the feature-rich self-service platform to Employers
- Improved sales by elevating the Employer and Member experience
Year 03
Year 03
Initiatives :
- Successfully deployed modern, revamped Broker and Provider Experience
- Stabilized new technologies by effectively managing high volumes of business on newly implemented platforms
- Developed a range of tools to streamline business processes, improve efficiency and reduce manual effort & execution time
Key Achievements
- Minimized manual intervention across multiple business processes, resulting in faster turnaround times and increased reliability
- Positioned EBMS as an innovation driven service provider that offers a modern, data-rich, and feature-rich experience for all stakeholders thereby, solidifying it’s market position
- Further reduced the call volumes by offering self-service capabilities to providers, enabling them to access information and execute transactions independently, without the need to contact the support center
Year 04
Year 04
Initiatives :
- Successfully deployed modern, revamped CSR Experience
- Integrated GPA TPA within the umbrella of Imagine360 across all stakeholder experience applications
Key Achievements
- Reduced call handling time for CSRs by eliminating the need to switch between multiple systems for information and actions
- Enabled EBMS to offer a dedicated CSR persona that allowed it’s customers to operate their own contact centers on the platform
- Seamlessly transitioned GPA TPA’s stakeholders from legacy systems to EBMS’ white-labeled portal, providing them with enhanced data access and a modern, intuitive experience
- Achieved cost savings by decommissioning GPA TPA’s legacy platforms
Year 05
Year 05
Initiatives :
- Revamped Member Experience to address the business need for a single integrated platform across all companies
- Developed new Enterprise APIs that integrate with diverse claim systems across the Imagine360 network of companies
- Built state-of-the-art admin portal platform that empowered the business to configure new groups and manage renewals independently, without requiring assistance from technology teams
Key Achievements
- Enterprise APIs established a unified access point to multiple claims systems across all group companies, creating a strong foundation for scalable enterprise-wide technology solutions
- Revamped Member Experience, built on the latest technology stack and powered by Enterprise APIs, enabled a seamless and centralized experience for customers utilizing services across multiple group companies
- The new Admin Portal significantly accelerated group onboarding, reducing the time from several days to just a few hours, driving business growth without the need for additional staff
Year 06
Year 06
Initiatives :
- Migrated a large volume of business to offer new Member Experience, and enabled speedy configurations using the admin portal
Key Achievements
- Ensured a smooth transition for users while migrating a large volume of business to the new Member Experience
- Facilitated a rapid setup and reduced time-to-market for groups by expediting configuration processes through the Admin Portal>
As a trusted, long-term technology partner of EBMS, we are deeply committed to continuously enhancing user experiences, streamlining operational processes, and modernizing systems. By aligning technology with their strategic objectives, we empower EBMS to seamlessly adapt to market changes, improve stakeholder engagement, and bring their business vision to life.
If you can introduce your business vision to us,
We can realize it with speed & perfection
