
The year is 2026. A member reaches out with a simple coverage question, expecting a fast, personalized response. But your systems lag—still reliant on outdated, disconnected tools that don’t communicate effectively.
Now consider your competitor. Their systems are fully integrated, giving agents real-time access to member data across all touch-points. They respond faster, more accurately, and with greater confidence.
This shift toward a modern, connected healthcare IT ecosystem is more than just a trend—it’s a strategic shift backed by market momentum. The healthcare IT integration market is projected to grow from $4.79 billion in 2024 to $5.31 billion in 2025—a 10.8% increase in just one year.
Driving this shift are several critical factors: rising operational costs, increasing pressure to enhance member experiences, and the growing need for data-driven, agile decision-making across the enterprise.
Yet many healthcare insurance enterprises still rely on disconnected systems—where data is siloed, tasks are manual, and member experiences fall short of expectations. The way forward lies in adopting connected, secure, and scalable technology solutions. By implementing integrated healthcare IT solutions, enterprises can unify data across systems, automate routine tasks, enable secure, real-time access to information, and deliver the personalized, efficient experiences today’s members expect.
This blog explores the common challenges integration can solve for insurers, the broader business impact of adopting integrated healthcare IT, and best practices to future-proof healthcare operations in an increasingly evolving digital environment.
Curious about how integrated healthcare IT solution providers can boost efficiency, reduce costs, and enhance member satisfaction? Let’s dive in.
Common Challenges in Healthcare IT Integration for Payers
Healthcare insurance is inherently complex. Yet, when systems within an enterprise operate in isolation, this complexity often transforms into significant operational inefficiencies. For insurers, these disconnected systems are more than just an IT issue—they represent a critical business challenge.
As pressures mount to optimize costs, ensure regulatory compliance, and deliver exceptional member experiences, fragmented data and disparate tools create obstacles that hinder even the most capable teams.
Integrated IT solutions for healthcare offer a way forward by breaking down silos and streamlining workflows. Below, we’ll explore the common challenges healthcare insurers face—and how integration can serve as a powerful catalyst for transformation.
1. Data Silos
While internal teams work hard to deliver results, the systems they rely on often operate in isolation. Many legacy platforms were built for specific departmental functions rather than enabling enterprise-wide collaboration. As a result, data becomes trapped within silos, creating bottlenecks that delay key processes—from claims adjudication to member support—ultimately reducing efficiency and diminishing the overall member experience.
2. Lack of Standardization
Healthcare systems often use a variety of data formats—such as EDI, HL7, or FHIR—which can lead to incompatibility across platforms. When systems can’t speak the same language, mismatches, errors, and delays become common. The absence of data standardization complicates internal collaboration, ultimately undermining both efficiency and care delivery.
3. Complex Ecosystems
Healthcare insurers operate within a broader ecosystem that includes providers, TPAs, labs, and other partners—each utilizing different tools and processes. A lack of seamless connectivity across this ecosystem results in operational friction and disrupts the delivery of consistent, high-quality member experiences.
4. Evolving Regulatory Requirements
Healthcare insurers must navigate a complex and ever-changing regulatory landscape, including standards set by HIPAA, CMS, and other governing bodies. Legacy systems often struggle to adapt quickly to new rules, creating compliance risks and operational slowdowns. Without integrated, up-to-date healthcare IT solutions, insurers face challenges in maintaining data security, audit readiness, and process agility—further straining resources and diverting focus from member-centric initiatives.
5. Security And Privacy Risks
With healthcare data among the most sensitive and highly regulated, insurers face mounting challenges in safeguarding member information. As systems multiply and integrations expand, the risk of breaches and unauthorized access grows. Legacy infrastructure often lacks the security agility needed to keep pace with evolving threats. Without a unified, secure IT framework, enterprises struggle to maintain compliance and protect member trust—placing both reputational and operational stability at risk.
6. Data Quality Issues
Accurate, timely data is the backbone of effective healthcare operations—but many insurers struggle with outdated or inconsistent information across systems. Errors in provider directories, member eligibility, or claims data can lead to compliance violations, administrative delays, and poor member experiences. Without integrated IT solutions for healthcare, insurers face ongoing challenges in delivering reliable, efficient, and compliant services.
7. Latency in Data Exchange
Timely access to accurate information is essential for responsive and effective decision-making. However, many healthcare systems rely on batch processing or delayed data transfers, which hinder real-time insights and slow down core operations. This latency impacts everything from claims processing to member support, resulting in missed opportunities, inefficiencies, and diminished member satisfaction. Integrated systems enable faster, more seamless data exchange—helping insurers stay agile and responsive in a fast-moving environment.
8. High Integration Costs
Many insurers rely on custom-built integrations and patchwork solutions to connect legacy systems and third-party tools. These efforts often require significant time, resources, and ongoing maintenance—diverting focus from strategic priorities. As IT teams juggle vendor coordination and system upkeep, costs escalate while value remains limited. Without scalable, purpose-built healthcare IT solutions, insurers face growing operational burdens that hinder innovation and strain budgets.
How Healthcare IT Solution Integration Benefits Insurance Operation
Imagine a healthcare insurance enterprise where teams are burdened by manual processes, member data is siloed across disconnected systems, and new product launches take months of cross-functional coordination. For many organizations, this isn’t a hypothetical situation —it’s the current reality.
System fragmentation is more than just an IT challenge; it’s a fundamental business barrier. The solution lies in integration : a strategic enabler that reduces complexity, accelerates time to market, and drives enterprise-wide efficiency and performance.
When done right, integration does more than connect systems. It accelerates data flow, enables faster decision-making, and empowers both teams and members with smoother, more responsive experiences. In a fast-moving healthcare insurance industry, effective integration is what keeps an enterprise agile—and ahead.
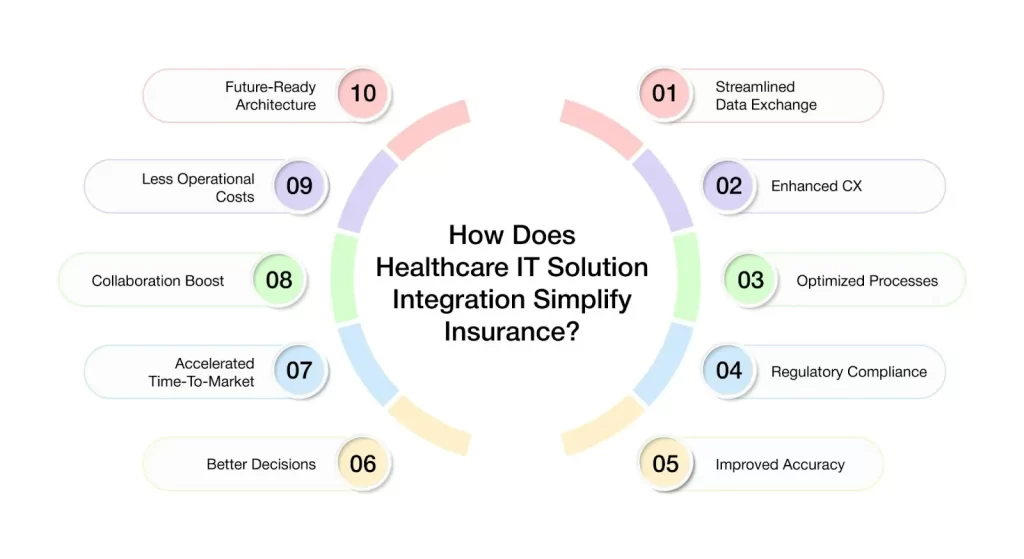
Below are the key benefits that demonstrate why integration is critical to optimizing insurance operations:
1. Streamlined Data Exchange
Integration enables real-time, secure data exchange across systems—from eligibility verification and claims adjudication to provider data management. By eliminating manual handoffs and data silos, insurers can reduce delays, minimize errors, and improve operational efficiency. Seamless information flow between internal teams and external partners ensures faster processing, improved accuracy, and a more connected member experience.
2. Enhanced Member Experience
Integration improves the member journey by enabling faster, more accurate interactions across touchpoints—from claims processing and eligibility checks to provider access and support services. With unified data and seamless system connectivity, members experience fewer delays, clearer communication, and quicker resolutions. The result is a smoother, more personalized experience that builds trust, strengthens engagement, and drives long-term loyalty.
3. Optimized Business Operations
Disconnected systems often lead to redundant work, higher administrative costs, and strained resources. Integration addresses these inefficiencies by automating routine tasks, reducing manual intervention, and streamlining workflows across functions. By eliminating duplication and improving coordination, insurers can increase productivity, control costs, and enable teams to focus on higher-value initiatives that drive business growth.
4. Simplified Regulatory Compliance
Staying compliant with evolving regulations—such as HIPAA, CMS guidelines, and state-specific mandates—can be challenging, especially with fragmented systems. Integrated solutions streamline compliance by embedding automated checks, ensuring data accuracy, and maintaining consistent documentation across processes. This not only reduces the risk of costly errors and audits but also enables insurers to adapt quickly to regulatory changes with confidence and efficiency.
5. Improved Data Accuracy & Consistency
Manual data entry and disconnected systems often lead to inconsistencies, outdated information, and costly errors. Integration centralizes data across platforms and ensures real-time synchronization, reducing the risk of duplication or inaccuracies. With accurate, up-to-date information readily available, insurers can strengthen critical processes like underwriting, renewals, and member assistance—leading to better decisions and more reliable outcomes.
6. Better Decision-Making
Disparate systems limit visibility, making it difficult to identify patterns, track performance, or respond effectively. Integration brings data together into a single, unified view—empowering leaders with real-time insights across operations, members, and markets. With comprehensive, reliable data at their fingertips, decision-makers can act faster, plan strategically, and drive better outcomes for both the business and its members.
7. Accelerated Time-to-Market
Bringing new plans or product features to market is often slowed by disconnected systems and complex technical dependencies. Integration streamlines development and deployment by reducing system friction and automating key processes. With fewer delays and greater agility, insurers can respond more quickly to market shifts, regulatory updates, and evolving member needs—launching innovations in weeks instead of quarters.
8. Improved Partner Collaboration
Healthcare insurers operate within a complex ecosystem of providers, TPAs, PBMs, brokers, and government agencies—each relying on timely, accurate data to deliver services. Integration enables seamless data exchange and coordination across these external partners, reducing friction and enhancing collaboration. The result is more efficient operations, improved care coordination, and a better overall experience for both members and healthcare stakeholders.
9. Reduced Operational Costs
Manual processes, paper-based workflows, and patchwork system fixes all contribute to rising operational costs. Integration reduces these inefficiencies by automating routine tasks, eliminating redundancies, and streamlining system interactions. By lowering administrative overhead and minimizing error-related expenses, insurers can reallocate resources toward innovation, growth, and delivering higher-value member experiences.
10. Future-Ready Architecture
A well-integrated IT ecosystem lays the foundation for long-term scalability and innovation. By connecting core systems and ensuring data flows seamlessly, insurers can more easily adopt emerging technologies—such as AI, advanced analytics, and evolving care models. Integration positions enterprises to adapt quickly, innovate confidently, and remain competitive in a rapidly changing healthcare landscape.
Proven Strategies for Successful Healthcare IT Integration
Integration is not just about connecting systems—it’s about enabling smarter operations across the enterprise. However, achieving success requires more than technology alone. It demands strategic planning, disciplined execution, and alignment across teams.
To realize the full value of integration—accelerated decisions, improved service delivery, and stronger compliance—the following best practices serve as essential steps on the path to transformation.
1. Adopting Industry Standards
Leveraging widely accepted healthcare data standards such as EDI, HL7, and FHIR is a foundational step toward effective integration. These standards promote interoperability, enabling seamless communication between internal systems and external partners—including providers, PBMs, TPAs, and government exchanges. Standardization not only streamlines onboarding and data exchange but also enhances data accuracy, consistency, and scalability across the healthcare ecosystem.
2. Implementing a Central Integration Platform
Establishing a centralized integration platform—such as VIZCare Connect—serves as a unified hub for managing data flows across diverse systems. By consolidating interfaces and automating data exchange, it reduces complexity, eliminates redundancies, and ensures consistent, real-time connectivity between internal teams and external partners. A central platform enhances operational efficiency, improves data accuracy, and enables teams to collaborate more effectively across the organization.
3. Prioritizing Data Governance
Successful integration depends on the quality and reliability of the data being exchanged. Establishing robust data governance practices ensures that data is accurate, secure, and compliant with regulatory requirements. This involves clearly defining data ownership, implementing quality control processes, and maintaining traceability of data sources. Strong governance not only supports regulatory readiness for audits such as HIPAA but also builds confidence in decision-making across clinical, operational, and administrative teams.
4. Enabling Real-Time Data Exchange
Timely access to accurate information is critical for responsive decision-making and service delivery. Implementing real-time data exchange capabilities allows insurers to process claims, verify member eligibility, and respond to service requests without delay. By moving beyond batch processing, enterprises can reduce latency, enhance member satisfaction, and increase operational agility—ultimately improving both efficiency and experience across the value chain.
5. Incorporating a Rules Engine
Integrating a rules engine into the IT infrastructure helps an enterprise enforce business logic and automate exception handling across workflows. By validating data exchanges in real time and managing rule-based conditions automatically, a rules engine reduces manual intervention, minimizes errors, and accelerates processing times. This not only increases operational reliability but also enhances scalability by supporting high-volume data exchanges with greater consistency and control.
6. Investing in Security and Compliance
Protecting sensitive healthcare data is fundamental to successful integration. Implementing robust security measures—such as end-to-end encryption, role-based access controls, and detailed audit logging—helps safeguard data throughout its lifecycle. These practices not only support compliance with regulations like HIPAA but also foster trust among members, external partners, and regulators. A proactive approach to security reduces risk exposure, ensures audit readiness, and reinforces the integrity of all integrated systems.
7. Enabling 360° Entity Views
Achieving a comprehensive view of key entities—such as members, providers, claims, and employers—is essential for delivering informed, personalized, and coordinated services. Integrated systems consolidate data from multiple sources to create a unified, real-time profile of each stakeholder. This holistic visibility empowers teams to improve care coordination, enhance service delivery, and make more strategic, data-driven decisions across the enterprise.
8. Fostering Cross-Functional Collaboration
Successful integration requires close collaboration across IT, operations, compliance, and business teams. Engaging key stakeholders from the outset ensures that technical capabilities align with business objectives, regulatory requirements, and user needs. This cross-functional alignment streamlines implementation, reduces miscommunication, and promotes broader adoption—ultimately leading to more effective and sustainable integration outcomes.
9. Monitoring and Optimizing Integration Performance
Integration is not a one-time initiative—it requires ongoing oversight to remain effective. Implementing continuous monitoring through performance dashboards, system logs, and automated alerts allows enterprises to proactively identify issues, track service-level agreements (SLAs), and fine-tune processes in real time. This commitment to continuous optimization ensures sustained efficiency, reduces downtime, and supports the long-term success of integrated operations.
AVIZVA: The Future of Healthcare IT Solutions for Insurers
AVIZVA is a healthcare technology company that empowers payers, TPAs, and PBMs to enhance care delivery through a comprehensive suite of engineering products and services. With over 14 years of experience in leveraging technology to simplify, optimize, and accelerate care, AVIZVA has become a trusted technology partner to a wide range of healthcare enterprises.
AVIZVA’s healthcare offerings are grouped into two key categories: Engineering Services and its proprietary product suite, VIZCare. Each product within VIZCare is purpose-built to address specific business challenges in healthcare.
A flagship product in this suite is VIZCare Connect – a robust, enterprise-grade data connectivity platform designed to address the end-to-end data integration and interoperability needs of healthcare enterprises. It provides a seamless, real- time data ecosystem, ensuring consistent, accurate, and accessible healthcare data across internal systems, external partners, and regulatory bodies.
Following are the key features of VIZCare Connect:
1.Data Orchestration and Synchronization
The platform supports a wide range of integration protocols and formats, automates complex data flows, and leverages built-in AI to dynamically configure sources, map fields, and optimize transformations.
- Ensures real-time data synchronization across internal systems and external stakeholders such as clearinghouses, providers, PBMs, payers, and regulatory bodies. It eliminates data silos and ensures accurate, up-to-date information across all touchpoints.
- Flexible Data Exchange: Supports multiple integration protocols and formats to accommodate diverse system requirements, including file-based EDI (Electronic Data Interchange), direct database interfaces, modern micro-services architecture with JSON structures and asynchronous event-based integration patterns for real-time updates and data consistency
- Automated Orchestration: Includes a workflow-driven, configurable data orchestration engine, eliminating manual intervention and ensuring timely, accurate data movement across all systems. Facilitates seamless data transformation, enrichment, and validation before reaching target systems.
- Built-in Rules Engine: Native rules engine enables dynamic data transformation, allowing seamless conversion from one format to another based on business logic and integration requirements.
2. A Comprehensive Healthcare API Suite
In today’s digital-first healthcare ecosystem, seamless connectivity and interoperability are essential. A modern, scalable, and secure API layer is not just a technical necessity but a business enabler, powering integrations, workflows, and application-driven use cases across an enterprise.
VIZcare’s Healthcare APIs are designed to support both real-time integrations and business process execution, ensuring that data flows effortlessly across internal and external systems while maintaining security, compliance, and operational efficiency.
- Comprehensive API Suite: A rich set of 300+ APIs that support lookup, read, search, add, and update functions across all healthcare data types. Designed to facilitate seamless integration across multiple applications and platforms.
- Built-in Business Logic & Real-World Workflow Support: APIs incorporate business rules, data interdependencies, and healthcare-specific logic, ensuring accurate, context-aware transactions. Supports transaction integrity across payer, provider, and regulatory ecosystems.
- Interoperability & Compliance: Includes all HL7 FHIR APIs, enabling CMS interoperability and compliance with federal regulations. Ensures secure, structured data exchange across healthcare networks, payers, and regulatory bodies.
3. Preloaded & Continuously Updated Healthcare Industry Data
VIZcare Connect’s preloaded, continuously updated healthcare datasets provide a foundation for data validation, reconciliation, and enrichment. By seamlessly integrating trusted industry data sources, Connect eliminates the need for complex, manual data ingestion processes, ensuring that healthcare organizations can operate with the most accurate and up-to-date information available.
Key datasets include: Provider Directories, Healthcare Codes (ICD, CPT, HCPCS, NDC, etc.), Networks & Pricing Information etc.
- Provider Data (Practitioners & Facilities):
- National Provider Identifiers (NPIs)
- Practitioner Taxonomies & Specialties
- Practice Locations & Contact Details
- Affiliations & Hospital Privileges
- Medicare & Medicaid Participation Status
- Credentialing & Licensing Information
- Healthcare Code Sets (Standardized Medical, Billing, and Drug Codes):
- CPT (Current Procedural Terminology) – Standard codes for medical services & procedures.
- ICD-10 (International Classification of Diseases) – Diagnostic codes for medical conditions.
- HCPCS (Healthcare Common Procedure Coding System) – Standardized coding for medical supplies, equipment, and services.
- DRG (Diagnosis-Related Groups) – Used for hospital reimbursement and case-based payments.
- NDC (National Drug Code) – Identifiers for prescription and OTC medications.
- GPI (Generic Product Identifier) – Hierarchical drug classification system for pharmacy claims processing.
- Network Data (Payer & Provider Network Information):
- National PPO
- Regional PPO
- Provider Directory
- Pricing, Contract & Transparency Data
Conclusion
In today’s rapidly evolving healthcare landscape, maintaining a competitive edge requires more than adaptation—it demands leadership. For insurers, that begins with intelligent, connected healthcare IT solutions that eliminate data silos, streamline operations, and deliver measurable value to both the enterprises and its members.
AVIZVA helps insurers realize this vision with VIZCare Connect – a robust, feature-rich platform that seamlessly connects legacy healthcare systems with modern real-time data platforms, ensuring secure, efficient, and interoperable data management. Discover what AVIZVA can do for your business—Schedule your strategy call today.

FAQs
1. What are the top healthcare IT companies driving digital transformation in 2026?
The top healthcare IT solutions providers in 2026 include companies that manufacture innovative IT solutions for the healthcare industry in the areas of data management, workflow improvement, and member care. Companies such as AVIZVA, Cerner, Allscripts, and several more companies are carrying out digital health transformation with most modern technologies in health interoperability solutions and cloud-based platforms.
2. How are healthcare IT companies improving member care and operational efficiency?
Healthcare IT solutions, when implemented well, ensure quality care by bringing efficiency to healthcare operations. They automate administrative duties, pass data real-time, and use AI and analytics to make better decisions. Therefore, with higher levels of automation across workflows and in collaboration, as well as user-level data access, healthcare IT solutions shall guarantee better health outcomes at lower operational costs.
3. What technologies are healthcare IT companies using to innovate healthcare services?
Healthcare IT companies are using AI-powered platforms, unified digital systems, secure interoperability tools, pre-built API suites, and continuously updated healthcare datasets to innovate services. These technologies streamline operations, improve data accuracy, enhance member engagement, and deliver faster, more personalized healthcare experiences.
4. How do healthcare IT solutions help healthcare providers comply with regulations?
Healthcare IT solutions and services assist healthcare providers in maintaining their compliance with regulatory agencies such as HIPAA and GDPR by automating data security protocols, thereby guaranteeing that data exchanges are performed in a secure manner, and easing the documentation process.
5. What are the key trends in healthcare IT to watch in 2026?
A 2026 key healthcare IT trend will be the emergence of AI-driven predictive analytics, the increased uptake of healthcare interoperability solutions, smart hyperautomation, cloud-based EHRs, and digital-first member experiences. The use of these technologies will positively affect care, healthcare operational efficiency, and regulatory compliance in healthcare altogether.
